Why trust, leadership, and culture are important safety tools
Over the past decade, the UK has seen a significant shift towards prioritising patient safety. Increased staffing, dedicated funding, and the introduction of patient safety specialists have all been positive steps. Yet despite these initiatives, progress in improving patient safety outcomes has remained relatively small (Government Review of Patient Safety, 2025).
So, what’s missing?
Emerging research and practical experience across both maternity and general healthcare point to the same themes again and again — trust, leader behaviour, and team culture.
What Defines a Positive Patient Safety Culture?
A positive patient safety culture is one where people feel safe to speak up — not just when things go wrong, but when they sense something might go wrong. It’s where curiosity replaces fear, and compassion replaces blame.
According to the Nuffield Trust, a strong safety culture includes:
- Value and respect for diversity
- Strong leadership and teamwork
- Openness to learning
- Psychological safety — an environment where individuals feel they’ll be treated fairly and compassionately if they raise a concern
When psychological safety is present, healthcare teams are more willing to report incidents, share learning from near misses, and escalate concerns early. It creates a climate of openness — essential for preventing harm and improving patient outcomes.
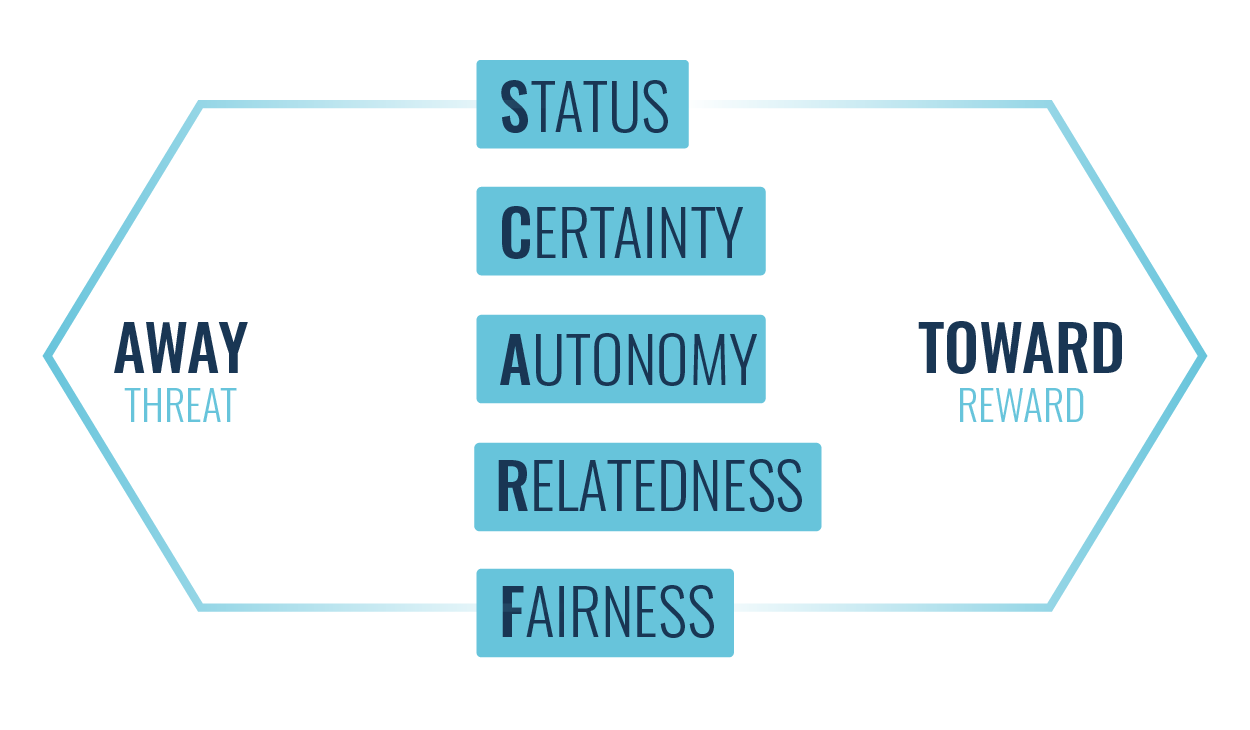
Why Psychological Safety Matters in Healthcare
Healthcare is inherently high-stakes and high-pressure. The expectation to perform perfectly under stress can make it difficult for staff to admit mistakes or voice uncertainty.
Psychological safety changes that dynamic. It’s the shared belief that it’s safe to speak up — that questions, feedback, and even dissent are welcomed rather than punished.
Research shows that in healthcare settings, psychological safety directly influences:
- Proactive behaviours, such as asking questions or sharing ideas (Ito et al., 2021)
- Error reporting and learning from mistakes (Leonard et al., 2015)
- Team communication and decision-making under pressure
When staff feel psychologically safe, they are more engaged, collaborative, and solution-focused. The result? A safer environment for both staff and patients.
How to Create a Positive Patient Safety Culture
Building a culture of safety doesn’t happen through policy alone — it’s about the daily behaviours, conversations, and values that shape how teams work together. Here are the key components:
1. Leadership Commitment
Leadership sets the tone for everything that follows. When leaders consistently demonstrate that safety is a core organisational value, not just a compliance measure, it creates clarity and confidence across teams.
Research highlights that effective leadership is crucial in shaping safety attitudes and building trust (Huang et al., 2024). The most influential leaders are those who:
- Model calm, compassionate responses when concerns are raised
- Listen before reacting, showing appreciation for staff speaking up
- Acknowledge their own uncertainty or mistakes, demonstrating vulnerability
- Recognise and reward proactive safety behaviours
Leadership isn’t just about setting direction — it’s about creating emotional safety for others to follow.
2. Open Communication and Psychological Safety
Encouraging open dialogue about mistakes, risks, and improvements requires trust and empathy. Implement short debriefs and opportunities to ask questions and raise concerns on ward rounds and hand-overs. Staff must believe that speaking up won’t lead to blame or punishment.
Leaders and managers can foster this by:
- Replacing “Who caused this?” with “What can we learn from this?”
- Starting meetings by inviting input from quieter voices
- Publicly appreciating people who raise concerns early
- Modelling curiosity instead of criticism
These small, consistent actions build psychological safety over time. And when that happens, the quality of communication — and therefore the quality of care — improves dramatically.
3. Continuous Learning and Improvement
A positive safety culture views errors not as failures, but as opportunities for growth.
This means moving beyond reactive investigations to proactive learning systems. Regular safety culture assessments, staff feedback loops, and debriefs after critical incidents help identify patterns and prevent recurrence. Staff need to know that something is actually done as a result of them raising concerns, otherwise it can feel pointless.
Practical ways to strengthen learning include:
- Conducting “learning huddles” after incidents to share takeaways
- Encouraging staff to reflect on near misses without fear
- Sharing success stories of good catches and improvements
By making learning routine, not just reactive, healthcare teams normalise growth and resilience.
4. Teamwork and Collaboration
High-functioning healthcare teams rely on clear communication, mutual respect, and shared goals.
Interprofessional teamwork — between nurses, doctors, allied health professionals, and administrative staff — ensures that every voice contributing to patient care is heard.
Ways to strengthen collaboration include:
- Team-based training on communication and coordination
- Role clarity exercises that help teams understand each other’s responsibilities
- Inclusive decision-making, especially in complex cases
When teams collaborate openly, they not only prevent errors but also enhance morale and trust — two essential ingredients for safety.
5. Accountability with Compassion
While psychological safety means freedom from blame, it doesn’t mean freedom from accountability. Clear expectations, defined roles, and transparent systems ensure that everyone understands their responsibility for safety.
Effective accountability structures:
- Clarify who is responsible for what
- Provide support rather than punishment when things go wrong
- Reinforce that accountability is about learning, not shame
This balance between compassion and accountability strengthens trust and reinforces a culture of integrity.
The Human Heart of Patient Safety
Behind every safety protocol and policy is a person — a nurse balancing competing demands, a doctor making rapid decisions, a team trying to do their best under pressure.
Psychological safety in healthcare recognises this humanity. It allows professionals to bring their full selves to work — to speak up, collaborate, and learn without fear.
When leaders prioritise compassion, communication, and learning, they not only protect patients but also create workplaces where people thrive.
Key Takeaways
- Psychological safety is the foundation of effective patient safety culture.
- Leadership behaviour — calm, curious, and compassionate — shapes how safe people feel to speak up.
- Open communication and continuous learning turn mistakes into momentum.
- Teamwork and trust transform safety from a checklist into a shared value.
A psychologically safe workplace is a clinical necessity. Because when staff feel safe, patients are safe too.
If this resonates with you and your team, we offer training designed to help healthcare leaders build trust, communication, and psychological safety from the inside out.
Learn more here: neuroedgegrowth.co.uk/training